Before we get into non-surgical gum treatment, let’s clear up some vocabulary. We need to understand what gum disease is. We need to get an idea of what surgical treatment is about. Surgery is very commonly recommend by the mainstream.
The Vocabulary
We dentists and hygienists have really messed up communications in this area.
Gum disease ought to mean sickness of the gum tissues. Well, it does mean that. But we use the term carelessly. It also means the destruction of the normal anatomy that attaches a dental root to the bone and the destruction of the bone itself.
When talking among ourselves, we dental professionals are more precise. We use the term gingivitis to mean gum (only) disease. The anatomical term for the gums is gingiva. (pronounced JIN-jiv-uh.) When itis (code for inflammation) is tacked on to the end of the word it means inflammation of the gums. Inflammation is the body’s healing response to some sort of injury. The injury might be trauma, a burn or an infection. Lots of things.
When there is an attack on the fibres that attach a tooth to the bone and an attack on the bone itself, dentists and hygienists use the term periodontitis or periodontal disease. Perio means around or surrounding. Dont stands for tooth. Then, we have good old itis tacked on the end again. That still means that something is inflamed. However, when applied to breakdown of the structures suporting a tooth, it almost always implies that infection is involved.
The Ailments
Each of these conditions can occur without the other. However, it is rare indeed to find someone with periodontal breakdown who does not also have gingivitis.
Whenever you hear gum disease you need to determine whether the topic is gingivitis or periodontitis.
Gingivitis
Of the two conditions, gingivitis is relatively harmless and easy to reverse. By relatively harmless I mean that once it is gone, you can’t tell it ever existed. There is no physical destruction of the gingiva. That does not mean it is okay to ignore it.
Inflammation is the body’s response to physical insult or injury. That’s a good thing. It is an amazing thing. We need to be able to heal. We want to see: Injury → Inflammation → Healing → Healed (nothing remains inflamed.)
Chronic means continuing over a long time. If the gingiva is chronically inflamed, it means the body is “stuck” in the healing phase. Something is inflamed far too long. That is not a good thing.
To see why, try this: Think of the name of a medical condition or illness. Think of several. In a Google search box type the name of one of them and then a space. Now type the word inflammation. Hit Enter. Depending on how common or rare the malady is, you will get between hundreds or millions of hits. Inflammation is linked to the illness. It usually occurs first. That means that inflammation might play a role in causing the illness. That ought to move you to take gingivitis seriously. You ought to be concerned about any chronic inflammation – even if “everyone has it.”
Gingivitis looks like red, shiny, sometimes puffy or swollen gum tissue. Most of your gum tissue will be pink. But, very close to the teeth, and between the teeth, it will be red or purple. You will sometimes (or always) find that your gums bleed when you brush and especially when you floss. That is gingivitis. It may or may not be accompanied by destruction of the anatomical features which embed the teeth in the jaw.
Periodontal Disease (Periodontitis)
Periodontal disease is the breakdown of the structures (“bone and gristle”) that hold a tooth firmly in place in the jaw. As the embedding structure is destroyed, the teeth loosen and become unable to do their jobs. Such damage causes people to lose more teeth than decay does.
Imagine a fence post protruding from the ground. The post represents a tooth, and the ground the bone which provides a solid foundation for it. Now “summon” a torrential rainfall. Currents of water swirl aggressively around the post causing severe soil erosion to various depths. In some places it might even reach the bottom of the post. Now you know what breakdown of the dental supporting structure looks like.
Early supporting structure breakdown is difficult for a person to detect. It is hidden beneath the gingiva. It looks fairly normal and there is typically no pain. Considerable damage can occur to the bone embedding tooth roots without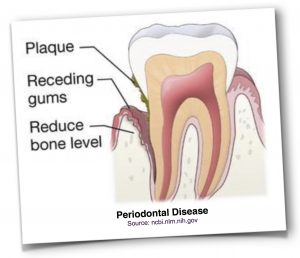 a person having any idea of something being wrong. It is very worthwhile to get an apparently healthy mouth checked to see if this is occurring. The process is usually painless until very late in the game.
a person having any idea of something being wrong. It is very worthwhile to get an apparently healthy mouth checked to see if this is occurring. The process is usually painless until very late in the game.
Advanced periodontitis is not so subtle. Teeth that are affected will have receding gingiva. (Don’t panic – by no means are all instances of receding gingiva a sign of loss of supporting structure.) There may be odour, pain and bleeding. If you push on a tooth, you might see it move. A (thankfully) obsolete term for advanced periodonitis is pyorrhoea. That translates as running pus. Charming.
Surgical Therapy
Surgical therapy for loss of dental supporting anatomy is offered by specialists in dentistry called periodontists. Any dental specialist has graduated as a general dentist and then taken an extra few years of training in their specialty.
“Destructive” Surgical Treatment
Until about twenty-five years ago all surgery targeting loss of dental embedding anatomy was essentially a destructive procedure. Ironically it causes even more loss by cuting away infected material and “re-landscaping” what is left to provide a terrain that the afflicted person can learn to “groom” and maintain in pristine condition. That is important because the nature of the destructive process is that it creates abnormally deep nooks and crannies (called pockets) where micro-oragnisms can breed and wreak havoc. Those nooks and crannies are very difficult or impossible to manage. The surgical solution? Cut them away.
“Traditional” Non-Surgical Treatment of Gum Disease
During that period of time I [Dr. McLean] was critical of the willingness of the profession to resort to this drastic treatment without first trying a comprehensive non-surgical gum treatment. Unfortunately the only non-surgical treatment for the mainstream was still a mechanical one – scaling and curettage. Scaling is mechanically scraping tartar off the teeth. Curettage is a somewhat more aggressive form of scaling where the intent is to remove not only the tartar and debris attached to the tooth, but the lining of the periodontal pockets that form there. The other traditional aspect of non-surgical gum treatment is educational – brushing and flossing instruction. That non-surgical program was and is well-intentioned and necessary but is insufficient in our experience.
In my mind, I likened this situation to the medical dilemma of necrotizing fasciitis (“flesh eating disease.”) Bacteria that are resistant to most antibiotics cause this nasty condition. That difficulty does not stop physicians from valiantly attempting to find an effective antibiotic. They prefer a non-surgical treatment. They try hard to solve the problem medically before they give up and resort to amputation of the affected limb. I know that’s not a fair comparison because amputation of an arm or a leg is not equivalent to “amputating” some of the anatomy surrounding the teeth.
Despite the unfairness of my comparison, the dental profession seems “trigger-happy” to me. They seem too eager to favour surgical over non-surgical treatment of the disease. The cynic in me suspects that may be because non-surgical approach commands a lower fee. Another reason may simply be that the non-surgical treatment they use has had disappointing results in the treatment of gum disease.
Reconstructive Surgical Treatment
During the last couple of decades periodontal surgery has progressed and there are now many situations where reconstructive surgical options exist. I have the same philosophical objection to that, except it is much less intense. The objective here is to restore – not destroy. That choice is often a good one, but I still believe that when a non-surgical therapy is feasible, then a non-surgical therapy ought to be done first. Choosing a minimally invasive option is the holistic way of doing things.
When the Patient is Passive, Failure is (Almost) Guaranteed
Both the reconstructive and what I term the destructive surgical corrections can result in a successful outcome. The success of either ultimately depends on a person reversing the conditions – by non-surgical means, obviously – that created the damage in the first place. Otherwise, return of infection and deterioration are extremely likely. Like most therapies that involve cutting, the patient’s responsibility is to show up and pay the bill. After all that is done he is told he needs to maintain his mouth in immaculate condition, quit smoking and change his diet. His role suddenly changes from passive to active. Sadly, it seems that often the sufferer doesn’t “get” the message and he assumes his new role rather half-heartedly. After a few years, when the malady has returned, a person will report, “The surgery didn’t take.”
Ironically, the ultmate success of the standard of care methods depends upon the patient’s adopting a holistic philosophy. She may not be aware that she has adopted this alternative view of things, but that is what needs to happen. She won’t call it alternative or holistic. She’ll call it common sense.
Three Treatments Compared
- To over-simplify at bit, if the appearance of loss of dental supporting arcitecture is to make a person “longer in the tooth,” the older (“destructive”) forms of surgery will expose more root surface to make the teeth appear even longer.
- The more recent (“reconstructive”) techniques can reverse some of that tissue loss and improve appearance.
- A non-surgical approach, in our experience will do neither of those things. To a great extent tissue will heal and bone defects hidden by the gingiva will fill in. But, the lost tissue will not grow back to hide the root surfaces that the destructive process has made visible. Nor do we have any theoretical expectation that it might. So non-surgical treatment has its limits.
If restoring the appearance of a mouth damaged by loss of dental supporting apparatus is the goal, reconstructive surgery is the best option.
Having said that, a wise first step is still doing a non-surgical treatment. Read especially Benefits of Non-Surgical Gum Treatment below.
Non-Surgical Gum Treatment
At last, we get to the point! There is no doubt that all destructive periodontal disease is infectious in nature. But even the mainstream recognizes there is more to it than that. The way this disease “behaves” suggests an exaggerated response to an irritant. It appears that the immune system’s overzealous attack against infecting organisms causes much of the gum and bone destruction that occurs. Much of the destruction is, so to speak, what the military would call “civilian collateral damage.”
That suggests that we should direct some therapy against the infecting organisms and make other efforts to “tame” a person’s response to the infection.
Empowering the Person
Here’s an example of how we think about such matters. You should realize that there is no formal research into our approach. It comes from trial and error from our practice and others who share our philosophy. We confront the problem, “How might we send a ‘cease fire’ message to the immune system?” We know that there are drugs that can do that, but they are dangerous and not approved for this clinical situation. We are not big fans of dangerous drugs.
The Example of Tuberculosis
The bacterium (tubercle bacillus) causing TB is a bit strange. Unlike many bacteria, it doesn’t seem to multiply wildly. It doesn’t produce toxins and invade tissue to cause damage and destruction. It just sort of sits there in the lung, minding its own business. Yet, people with TB have large areas of lung destruction surrounding colonies of tubercle bacilli. The “waxy” nature of the cell wall of that particular “bug” apparently makes our immune systems over-react. The destruction – the “disease” – is not caused by the infecting organism. We do the damage to ourselves with unrelenting attacks on the tubercle bacillus.
Vitamin D
We know from studying nutrition that Vitamin D is effective at fighting tuberculosis. Vitamin D does lots of things in the body. Building strong bones is a tiny fraction of its many roles. There are two things of interest here. First, we want to tell to the immune system to cease fire. Second, we want to tell our DNA to make some cathelicidin. That is a substance that fights infection – an antibiotic, if you will – intended by nature for use by our own bodies. Happily, Vitamin D sends both those messages for us.
Therefore, this clever molecule seems like something that ought to be useful in fighting periodontitis. Is there a reason that we should not go there? Is vitamin D dangerous? No. Does it have side effects? Hundreds of them and they are all good. Almost all of us are Vitamin D deficient and that alone is reason enough to utilize it.*
However, don’t imagine that I’m saying that vitamin D alone will rid you of periodontal disease. If only life were that simple! We have no solid evidence that Vitamin D affects periodontal disease at all. But, there are good reasons to think that it ought to help. This side trip into Vitamin D is just an example of how we devise our protocol. It is one of several supplements we suggest. Also, it is part of the lifestyle change we encourage a patient to adopt.
Targeting the Infection
Here’s what we suggest:
- Examine the plaque with a microscope and record what we see.
- Analyse your general health, medications, diet, and supplements.
- Record the condition of the tissue clinically and with x-rays.
- Now we know the starting conditions.
- Depending on what the microscope tells us, we start you on a home care regime of using natural products aimed at improving your general health and at attacking micro-organisms.
- Most of the time, the microscope will show the presence of amoeba or other protozoa in the plaque. The mainstream is only concerned about bacteria.
- Our experience is that when the protozoa disappear, healing starts.
- The microscope guides decisions about what to do next as much or maybe more than clinical findings do.
- Our experience over the years tells us to postpone mechanical debris removal (scaling) until the infection has lessened (unless there is some strong reason to do otherwise.) Sometimes, when we “jump in” to to clean up the area too soon, patients complain of feeling ill afterwards, and the mouth becomes very sore. The message we take away from that is “Stop jumping in so soon.”
Is This Non-Surgical Treatment of Gum Disease Holistic?
- Those folks who seek alternative dental services frequently enquire about non-surgical treatment of gum disease. Because this approach is a far less invasive form of periodontal therapy, the holistic (alternative) community is drawn to it.
- We use natural products as an alternative to drugs except in unusual circumstances. The object of therapy is not to destroy all the micro-orgaisms of the mouth. Instead we do what we can to establish healthy ecology – a normal balance of micro-oganisms. One body part living in a healthy relationship with another is a holistic concept. It’s an appealing alternative to “drugging a body part into submission.”
- Using vitamins, supplements and dietary choices to encourage healing is certainly a holistic alternative to relying on mechanics and medicine.
- The body wants to heal. There are limits, however, to what can occur naturally. I don’t think there are any in the holistic (alternative) community who fail to see the wisdom of reducing (“setting”) a broken arm so that it can heal. If the bony fractured ends don’t contact each other, the pieces won’t knit together. Reducing a fracture is a mainstream (“allopathic”) procedure. But, our experience is that many periodontal defects that the mainstream assumes cannot heal without mechanical intervention, in fact do heal if conditions are right. We aren’t precisely sure how to define “right conditions.” We don’t have scientific studies from peer-reviewed journals to back us up. But, this alternative to the mainstream way of doing things often surprises us. Alas, occasionally it disappoints us. Then surgery is appropriate. Trying a non-toxic, safe, relatively inexpensive approach prior to a mainstream standard of care one is consistent with a holistic philosophy.
- Both the mainstream and the alternative communities share the notion that long-term success depends upon the afflicted peron’s deliberately taking responsibility for alternative lifestyle changes. Such a notion is an ancient holistic one – not a mainstream innovation.
Benefits of Non-Surgical Gum Treatment
- One major benefit of all this is that if success occurs, the patient’s experience is that the success is a result of what the patient did. Apart from professional scaling and perhaps irrigation of gum pockets, the patient performs the great majority of the therapy. Our role is to make suggestions and to keep score. If the patient knows she created the success, she also knows she can maintain the success.
- In a sense, what starts out as an intense protocol of tasks to perform evolves into a relaxed and comfortable lifestyle change. If your new habits support the maintenance of a healthy mouth, you will likely enjoy other seemingly unrelated changes for the better in your general health. That’s a holistic phenomenon. That’s what makes this kind of approach fun – the discovery of perhaps unexpected, but treasured “side effects.”
- The other benefits of this alternative approach is that it is less expensive than specialist care and much less uncomfortable than surgery.
- Even if reconstructive periodontal surgery had been planned from the beginning, it will now be done on healthy tissue. The patient will already be expert in maintaining the result.
- If some areas have “refused” to heal, more traditional (“destructive“) surgery will still be required. But, there will very likely be a need for less of it. Again, the patient will have already learned the lifestyle and habits necessary to maintain the result. That adjusting lifestyle habits can deliberatly affect health is a holistic concept – although the mainsteam probably doesn’t want to admit that.?
* There are people who need to be careful about Vitamin D intake. For instance, those with sarcoidosis are very sensitive to it and should take Vitamin D only under a physician’s supervision.
